TGA raids pharmacy for alleged fake weight-loss product manufacturing
By
Seia Ibanez
- Replies 13
As we manage our health and well-being with the utmost diligence, the importance of having access to safe and authentic medications is paramount.
That's why the recent news of a chemist raided for allegedly producing counterfeit medication is particularly troubling.
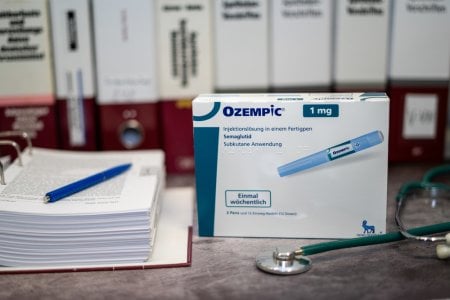
The Therapeutic Goods Administration (TGA) raided a pharmacy in South Yarra under suspicion of producing fake versions of the sought-after weight-loss medication, Ozempic.
In its statement, TGA said its agents executed a search warrant on the chemist on Thursday, 29 February, and seized documents and a ‘number of items which will be subject to further analysis and examination’.
Some items included semaglutide, a key ingredient in Ozempic, peptides, and human growth hormones, which the TGA alleged were illegally manufactured.
‘The TGA held serious concerns around the safety and efficacy of the medication if it were to be dispensed to the public,’ TGA said.
Australia has specific regulations governing the practice of compounding—the process by which pharmacies produce small quantities of drugs.
With the shortage of Ozempic, some pharmacies have reportedly resorted to compounded versions of Ozempic to treat patients diagnosed with type 2 diabetes.
While the practice is legal under controlled conditions, the allegations suggested that the South Yarra chemist may have crossed the line.
Professor Anthony Lawler, TGA head and Deputy Secretary of the Department of Health and Aged Care, has cautioned consumers and chemists about the repercussions of unlawful compounding.
‘It is important that pharmacists understand that they are most likely breaking the law if they are manufacturing or supplying medicines prior to receiving a prescription, except in very limited circumstances,’ he said.
‘Individuals and businesses, including pharmacists and pharmacies, must understand and comply with their legal obligations under the Therapeutic Goods Act 1989 with respect to the import, manufacture, advertising, supply or export of therapeutic goods.’
‘Consumers need to understand that the safety of compounded medicines [is] not assessed by the TGA, and they are not subject to the same controls over the quality or efficacy of the goods when compared with medicines approved for supply in Australia.’
Penalties for pharmacies that break the rules include fines and legal actions.
Ozempic supply won’t be enough this year due to the high demand for the drug as a weight loss product.
Aside from Ozempic, the TGA also issued an urgent warning late last year that the country is grappling with a critical shortage of over 400 medications, with over 60 said to shortly go into shortage at the time and over 250 already discontinued.
Although the TGA suggested Ozempic only for type 2 diabetes, many healthcare providers in Australia and abroad prescribe it to people who want to lose weight through ‘off-label’ prescribing.
In Australia, it's common for doctors to prescribe treatments outside those approved by the TGA, especially for rare diseases or underrepresented patient groups.
Despite the Ozempic shortage for people with type 2 diabetes, TGA can't control on decisions of health professionals, so they can’t prevent the limited supply from being used for weight loss.

What are your thoughts on this news? Let us know in the comments below!
That's why the recent news of a chemist raided for allegedly producing counterfeit medication is particularly troubling.
The Therapeutic Goods Administration (TGA) raided a pharmacy in South Yarra under suspicion of producing fake versions of the sought-after weight-loss medication, Ozempic.
In its statement, TGA said its agents executed a search warrant on the chemist on Thursday, 29 February, and seized documents and a ‘number of items which will be subject to further analysis and examination’.
Some items included semaglutide, a key ingredient in Ozempic, peptides, and human growth hormones, which the TGA alleged were illegally manufactured.
‘The TGA held serious concerns around the safety and efficacy of the medication if it were to be dispensed to the public,’ TGA said.
Australia has specific regulations governing the practice of compounding—the process by which pharmacies produce small quantities of drugs.
With the shortage of Ozempic, some pharmacies have reportedly resorted to compounded versions of Ozempic to treat patients diagnosed with type 2 diabetes.
While the practice is legal under controlled conditions, the allegations suggested that the South Yarra chemist may have crossed the line.
Professor Anthony Lawler, TGA head and Deputy Secretary of the Department of Health and Aged Care, has cautioned consumers and chemists about the repercussions of unlawful compounding.
‘It is important that pharmacists understand that they are most likely breaking the law if they are manufacturing or supplying medicines prior to receiving a prescription, except in very limited circumstances,’ he said.
‘Individuals and businesses, including pharmacists and pharmacies, must understand and comply with their legal obligations under the Therapeutic Goods Act 1989 with respect to the import, manufacture, advertising, supply or export of therapeutic goods.’
‘Consumers need to understand that the safety of compounded medicines [is] not assessed by the TGA, and they are not subject to the same controls over the quality or efficacy of the goods when compared with medicines approved for supply in Australia.’
Penalties for pharmacies that break the rules include fines and legal actions.
Ozempic supply won’t be enough this year due to the high demand for the drug as a weight loss product.
Aside from Ozempic, the TGA also issued an urgent warning late last year that the country is grappling with a critical shortage of over 400 medications, with over 60 said to shortly go into shortage at the time and over 250 already discontinued.
Although the TGA suggested Ozempic only for type 2 diabetes, many healthcare providers in Australia and abroad prescribe it to people who want to lose weight through ‘off-label’ prescribing.
In Australia, it's common for doctors to prescribe treatments outside those approved by the TGA, especially for rare diseases or underrepresented patient groups.
Despite the Ozempic shortage for people with type 2 diabetes, TGA can't control on decisions of health professionals, so they can’t prevent the limited supply from being used for weight loss.
Key Takeaways
- The Therapeutic Goods Administration (TGA) executed a search warrant on a chemist suspected of making fake Ozempic.
- A variety of medications, including semaglutide, peptides, and human growth hormones, were seized for further analysis.
- Professor Anthony Lawler from the TGA warned of serious consequences for chemists violating the Therapeutic Goods Act 1989.
- Supply shortages for Ozempic, primarily prescribed for type 2 diabetes, are being exacerbated by its off-label use for weight loss.