Should GPs bring up a patient’s weight in consultations about other matters? We asked 5 experts
- Replies 6
Australian of the Year and body positivity advocate Taryn Brumfitt has called for doctors to avoid discussing a patient’s weight when they seek care for unrelated matters.
A 15-minute consultation isn’t long enough to provide support to change behaviours, Brumfitt says, and GPs don’t have enough training and expertise to have these complex discussions.
'Many people in larger bodies tell us they have gone to the doctor with something like a sore knee, and come out with a ‘prescription’ for a very restrictive diet, and no ongoing support,' Brumfitt told the Nine newspapers.
By raising the issue of weight, Brumfitt says, GPs also risk turning patients off seeking care for other health concerns.
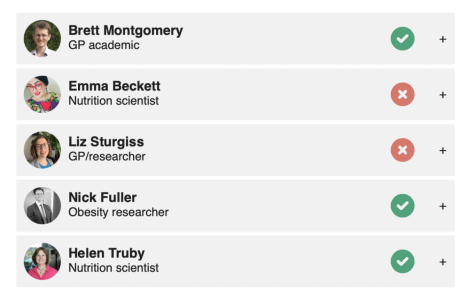
So should GPs bring up a patient’s weight in consultations about other matters? We asked 5 experts.
Brett Montgomery
GP Academic
Yes, sometimes – but with great care.
I agree that weight stigma is damaging, and insensitively raising weight in consultations can hurt people's feelings and create barriers to other aspects of health care.
I also agree people can sometimes be 'overweight' yet quite healthy, and that common measures and categories of weight are questionable.
On the other hand, I know obesity is associated with heart disease, joint problems, diabetes and cancers.
GPs should be ready to help people with their weight when they want help. Our assistance is somewhat effective, though sadly dietary efforts often have minimal effect on weight in the long term. Meanwhile, treatments causing larger weight changes (surgery and some medicines are often financially inaccessible.
I feel safe discussing weight when my patient raises the issue. Fearing hurting people, I often avoid raising it myself. I focus instead on health rather than weight, discussing physical activity and healthy diet – these are good things for people of any size.
Emma Beckett
Nutrition Scientist
No. It’s not likely to succeed. Large systematic reviews bringing together multiple studies of multiple weight-loss diets show weight loss is not generally maintained long term (12 months to four years).
The idea that weight is about willpower is outdated. The current body of evidence suggests we each have a weight set point that our body defends. This is determined by genetics and environment more so than education.
There may be associations between weight and health outcomes, but losing weight does not necessarily equate with improving health.
Fat stigma and fatphobia are harmful too and can compromise access to health care.
Instead, consider asking a better question. Healthy eating reduces disease risk regardless of weight. So maybe ask how many vegetables are your patients eating. Would they like to see a dietitian to discuss strategies for a better-quality diet?
Liz Sturgiss
GP/Researcher
No. A US study estimates it would take a family doctor 131% of their work hours to implement all preventive health-care recommendations. It's impossible to address every recommendation for preventative care at every consultation. One of the key skills of a GP is balancing the patient and doctor agenda.
Weight stigma can deter people from seeking health care, so raising weight when a patient doesn't have it on their agenda can be harmful. A strong therapeutic relationship is critical for safe and effective health care to address weight.
Weight is always on my agenda when there is unexpected weight loss. If a patient has rapid weight loss, I am concerned about an undetected cancer or infection. Additionally, I am increasingly seeing patients who are unable to afford food, who often have poor oral health, who lose weight due to poverty. Weight loss for the wrong reasons is also a very concerning part of general practice.
Nick Fuller
Obesity Researcher
Yes. GPs should play a role in the early detection of weight issues and direct patients to evidence-based care to slow this progression. Research shows many people with obesity are motivated to lose weight (48%). Most want their clinician to initiate a conversation about weight management and treatment options.
However, this conversation rarely occurs, resulting in significant delays to treatment.
Starting the conversation presents challenges. Although obesity is a complex disease related to multiple factors, it's still highly stigmatised in our society and even in the clinical setting. Sensitivity is required and the wording the clinician uses is important to make the patient feel safe and avoid placing blame on them. Patients often prefer terms such as 'weight' and 'BMI' (body mass index) over 'fatness', 'size' or 'obesity', particularly women.
Measuring weight, height and waist circumference should be considered routine in primary care. But this needs to be done without judgement, and in collaboration with the patient.
Helen Truby
Nutrition Scientist
Yes. A high body weight contributes to many chronic conditions that negatively impact the quality of life and mental health of millions of Australians.
Not all GPs feel confident having weight conversations, given the sensitive nature of weight and its stigma. GPs' words matter – they are a trusted source of health information. It’s critical GPs gain the skills to know when and how to have positive weight conversations.
GPs need to offer supportive and affordable solutions. But effective specialist weight management programs are few and far between. More equitable access to programs is essential so GPs have referral pathways after conversations about weight.
GPs' time is valuable. Activating this critical workforce is essential to meet the National Obesity Strategy's goals. But we need to fund primary care so GPs are remunerated for incorporating prevention discussions into consultations.
Disclosure statements:
Brett Montgomery is a general practitioner. He does not have a specific interest in obesity, but like almost all GPs, he treats many patients who are overweight or obese. He is a fellow of the Royal Australian College of General Practitioners; the college’s position statement on obesity prevention and management is linked to from this article. However, Brett writes here as an individual, and not on behalf of any organisation.
Emma Beckett has received funding for research or consulting from Mars Foods, NHMRC, ARC, AMP Foundation, Kellogg, and the University of Newcastle. She works for Nutrition Research Australia and member of committees/working groups related to nutrition or the Australian Academy of Science, the National Health and Medical Research Council and the Nutrition Society of Australia. Emma has lived experience of GPs bringing up her weight.
Liz Sturgiss receives funding from NHMRC, RACGP Foundation, National Centre for Healthy Ageing, Victorian Health Promotion Foundation. She is an appointed committee member of the Guidelines Development Committee for the review and update of the Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia and is the co-founder of the RACGP Specific Interest Group in Poverty.
Nick Fuller works for the University of Sydney and has received external funding for projects relating to the treatment of overweight and obesity. He is the author and founder of the Interval Weight Loss program.
Helen Truby has received funding from the NHMRC, the MRFF, the Commonwealth Department of Health, Health and Wellbeing Qld, Clinical Therapy Research in the Specialist Health Services (KLINBEFORSK, Norway), the Andrea Joy Logan Trust, the Victorian Cancer Agency Health Services Scheme.
This article was first published on The Conversation, and was written by Fron Jackson-Webb, Deputy Editor and Senior Health Editor.
A 15-minute consultation isn’t long enough to provide support to change behaviours, Brumfitt says, and GPs don’t have enough training and expertise to have these complex discussions.
'Many people in larger bodies tell us they have gone to the doctor with something like a sore knee, and come out with a ‘prescription’ for a very restrictive diet, and no ongoing support,' Brumfitt told the Nine newspapers.
By raising the issue of weight, Brumfitt says, GPs also risk turning patients off seeking care for other health concerns.
So should GPs bring up a patient’s weight in consultations about other matters? We asked 5 experts.
Three out of five said yes
Here are their detailed responses:Brett Montgomery
GP Academic
Yes, sometimes – but with great care.
I agree that weight stigma is damaging, and insensitively raising weight in consultations can hurt people's feelings and create barriers to other aspects of health care.
I also agree people can sometimes be 'overweight' yet quite healthy, and that common measures and categories of weight are questionable.
On the other hand, I know obesity is associated with heart disease, joint problems, diabetes and cancers.
GPs should be ready to help people with their weight when they want help. Our assistance is somewhat effective, though sadly dietary efforts often have minimal effect on weight in the long term. Meanwhile, treatments causing larger weight changes (surgery and some medicines are often financially inaccessible.
I feel safe discussing weight when my patient raises the issue. Fearing hurting people, I often avoid raising it myself. I focus instead on health rather than weight, discussing physical activity and healthy diet – these are good things for people of any size.
Emma Beckett
Nutrition Scientist
No. It’s not likely to succeed. Large systematic reviews bringing together multiple studies of multiple weight-loss diets show weight loss is not generally maintained long term (12 months to four years).
The idea that weight is about willpower is outdated. The current body of evidence suggests we each have a weight set point that our body defends. This is determined by genetics and environment more so than education.
There may be associations between weight and health outcomes, but losing weight does not necessarily equate with improving health.
Fat stigma and fatphobia are harmful too and can compromise access to health care.
Instead, consider asking a better question. Healthy eating reduces disease risk regardless of weight. So maybe ask how many vegetables are your patients eating. Would they like to see a dietitian to discuss strategies for a better-quality diet?
Liz Sturgiss
GP/Researcher
No. A US study estimates it would take a family doctor 131% of their work hours to implement all preventive health-care recommendations. It's impossible to address every recommendation for preventative care at every consultation. One of the key skills of a GP is balancing the patient and doctor agenda.
Weight stigma can deter people from seeking health care, so raising weight when a patient doesn't have it on their agenda can be harmful. A strong therapeutic relationship is critical for safe and effective health care to address weight.
Weight is always on my agenda when there is unexpected weight loss. If a patient has rapid weight loss, I am concerned about an undetected cancer or infection. Additionally, I am increasingly seeing patients who are unable to afford food, who often have poor oral health, who lose weight due to poverty. Weight loss for the wrong reasons is also a very concerning part of general practice.
Nick Fuller
Obesity Researcher
Yes. GPs should play a role in the early detection of weight issues and direct patients to evidence-based care to slow this progression. Research shows many people with obesity are motivated to lose weight (48%). Most want their clinician to initiate a conversation about weight management and treatment options.
However, this conversation rarely occurs, resulting in significant delays to treatment.
Starting the conversation presents challenges. Although obesity is a complex disease related to multiple factors, it's still highly stigmatised in our society and even in the clinical setting. Sensitivity is required and the wording the clinician uses is important to make the patient feel safe and avoid placing blame on them. Patients often prefer terms such as 'weight' and 'BMI' (body mass index) over 'fatness', 'size' or 'obesity', particularly women.
Measuring weight, height and waist circumference should be considered routine in primary care. But this needs to be done without judgement, and in collaboration with the patient.
Helen Truby
Nutrition Scientist
Yes. A high body weight contributes to many chronic conditions that negatively impact the quality of life and mental health of millions of Australians.
Not all GPs feel confident having weight conversations, given the sensitive nature of weight and its stigma. GPs' words matter – they are a trusted source of health information. It’s critical GPs gain the skills to know when and how to have positive weight conversations.
GPs need to offer supportive and affordable solutions. But effective specialist weight management programs are few and far between. More equitable access to programs is essential so GPs have referral pathways after conversations about weight.
GPs' time is valuable. Activating this critical workforce is essential to meet the National Obesity Strategy's goals. But we need to fund primary care so GPs are remunerated for incorporating prevention discussions into consultations.
Disclosure statements:
Brett Montgomery is a general practitioner. He does not have a specific interest in obesity, but like almost all GPs, he treats many patients who are overweight or obese. He is a fellow of the Royal Australian College of General Practitioners; the college’s position statement on obesity prevention and management is linked to from this article. However, Brett writes here as an individual, and not on behalf of any organisation.
Emma Beckett has received funding for research or consulting from Mars Foods, NHMRC, ARC, AMP Foundation, Kellogg, and the University of Newcastle. She works for Nutrition Research Australia and member of committees/working groups related to nutrition or the Australian Academy of Science, the National Health and Medical Research Council and the Nutrition Society of Australia. Emma has lived experience of GPs bringing up her weight.
Liz Sturgiss receives funding from NHMRC, RACGP Foundation, National Centre for Healthy Ageing, Victorian Health Promotion Foundation. She is an appointed committee member of the Guidelines Development Committee for the review and update of the Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia and is the co-founder of the RACGP Specific Interest Group in Poverty.
Nick Fuller works for the University of Sydney and has received external funding for projects relating to the treatment of overweight and obesity. He is the author and founder of the Interval Weight Loss program.
Helen Truby has received funding from the NHMRC, the MRFF, the Commonwealth Department of Health, Health and Wellbeing Qld, Clinical Therapy Research in the Specialist Health Services (KLINBEFORSK, Norway), the Andrea Joy Logan Trust, the Victorian Cancer Agency Health Services Scheme.
This article was first published on The Conversation, and was written by Fron Jackson-Webb, Deputy Editor and Senior Health Editor.
Last edited by a moderator: