Prostate Cancer: Aussie Dads and Grandads Are Talking About Their Health
- Replies 5
News of US President Joe Biden’s prostate cancer diagnosis hit headlines worldwide in May 2025.
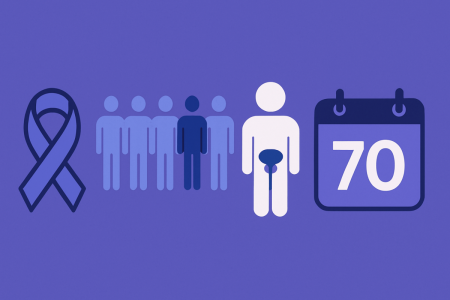
Back home, older Australians took notice — not because we have White House secrets, but because Biden’s situation reminds us that prostate cancer could touch us or our loved ones. In Australia, about one in six men will be diagnosed with prostate cancer by age 85, with the average diagnosis around age 70.
In fact, it’s already our most commonly diagnosed cancer (about 16% of all new cases) and the second-leading cause of cancer death in men. We’ve often brushed it off, but maybe we shouldn’t.
This friendly report mixes solid facts and real stories so that Aussie blokes 60+ can feel empowered — not scared — to discuss prostate health. Because sometimes, the best thing we can do is just talk.
When symptoms do surface, they often look like those of a benign enlarged prostate, not a screaming cancer siren. Watch for signs such as:
More serious warning signs (usually indicating spread) include persistent pain in the lower back, hips or legs, unexplained weight loss, or fatigue. If you have these, see a doctor immediately. Fortunately, most prostate cancers are caught before this stage these days.
A few risk factors to know:
Yes, there’s controversy. A Federal review (to report in 2025) is examining the benefits of different screening strategies. The 2016 guideline (still in force) says men aged 50–69 should have an informed discussion with their doctor about PSA testing every 2 years (sooner at age 45 if you have a strong family history). Over 70, routine PSA tests are usually discouraged unless you’re very fit.
For now, don’t let confusion stop you. If you’re over 50 (or 45+ and high-risk), simply ask your GP for a PSA test when you see them. It’s just a blood draw. As PCFA CEO Anne Savage warns, “prostate cancer often has no symptoms, and increasing numbers of men go untested, only to be diagnosed with late-stage and incurable disease”. In other words, having symptoms is not a prerequisite. Your doctor can explain the pros and cons and, if needed, arrange further tests (like an MRI or biopsy) before any treatment.
One more myth to bust: a raised PSA doesn’t automatically mean you have cancer. If your PSA is high, the next step is usually an MRI or a biopsy to find out what’s causing it. And if a biopsy is needed, modern techniques make it safer than ever (many specialists now use a transperineal approach, which greatly lowers infection risk). But again, those are just next steps – not an automatic scare. For now, a simple rule: if you’re unsure, talk to your GP. Having a PSA check every couple of years is a quick way to look after yourself.
And remember: metastatic (spread) prostate cancer is still treatable. It’s no longer an instant death sentence. In fact, as one Australian oncologist noted (citing US data), many men with advanced prostate cancer “can expect to live four or five years” even after it has spread. Men like Chris, mentioned below, show that these cancers can often be managed chronically. This isn’t to downplay it — just to reinforce that treatments today can keep men active for many more years than in the past.
We say it again: talk to someone. Your mate at the pub, the neighbor next door, or the woman in your life who keeps an eye out on you — start the chat. It could be over a coffee: “By the way, have you had your prostate checked yet?” Don’t be shy. In fact, a simple text can sometimes break the ice: “Hey mate, just had my check-up, all good. You might book yours soon!” Leading by example often works better than nagging.
If you’re the one feeling worried, consider involving those you trust. Many men report that it was their wife or partner who finally insisted on a check-up. Some even only went because their GP reminded them. Partners and friends notice things too (like more nightly bathroom trips) — let them help.
Medical help is there. The Cancer Council and PCFA have free helplines and resources. Support groups and counselling services are available. Australia’s hospitals now routinely offer psychological support for cancer patients, because it’s as much about mind as body. The point is: help is available, and you deserve it.
Our experts repeat: awareness and early action are the keys. We’ve done wonders raising awareness of women’s breast cancer — let’s do the same for ours. This is not about scaremongering; it’s about empowerment.
Movember’s Prostate Cancer Research Centre and government grants are pouring millions into finding new treatments. Last year PCFA reported prostate cancer now costs our health system over $1.35 billion each year and caused more hospital days than any other male cancer. That hefty cost is pushing more funding into better care and support for men.
In plain terms: Australians are not standing still. Every year brings better techniques, more effective drugs (like targeted immunotherapies), and more Aussie-led discoveries. This rising tide of research means that a prostate cancer diagnosis today has a far better outlook than a generation ago.
And don’t stop at yourself. The guy next door, the man at the grocery store with you, your son and grandson — anyone in their 50s or above — should hear about this too. Sometimes a simple text or message can do the trick: “Hey mate, just had my check-up, all good. You might book yours soon!” Leading by example often works better than nagging.
Our experts say awareness and early action are the keys. So, who will you start that conversation with today?
Disclaimer: Always consult a healthcare professional with any health concerns or before making changes to your medication, diet or exercise routine. This article is intended for general information only and does not replace medical advice.
Back home, older Australians took notice — not because we have White House secrets, but because Biden’s situation reminds us that prostate cancer could touch us or our loved ones. In Australia, about one in six men will be diagnosed with prostate cancer by age 85, with the average diagnosis around age 70.
In fact, it’s already our most commonly diagnosed cancer (about 16% of all new cases) and the second-leading cause of cancer death in men. We’ve often brushed it off, but maybe we shouldn’t.
This friendly report mixes solid facts and real stories so that Aussie blokes 60+ can feel empowered — not scared — to discuss prostate health. Because sometimes, the best thing we can do is just talk.
The Numbers You Need to Know
- 26,400 Australian men will be diagnosed in 2024. That’s nearly 72 men every day — roughly one in five men over a lifetime. (It’s largely a disease of older men: around 72% of cases are in those aged 60–79, and the median age at diagnosis is about 69.)
- Nearly 3,900 Australian men will die from it in 2024 (about 11 men a day). It causes roughly 13% of cancer deaths in men. Anne Savage of the Prostate Cancer Foundation of Australia (PCFA) calls this toll “tremendous” and says it’s “an unacceptable price to pay” for a disease that is often treatable if caught early.
- Survival rates are high if caught early. About 95.8% of men survive at least five years after diagnosis (and 91% reach 10 years). Over 250,000 Australian men are alive today after a prostate cancer diagnosis in the past four decades. Experts note that if every man were diagnosed at the earliest stage and given modern treatment, “we can beat this disease”.
- It’s a disease of older men. Almost no one under 50 gets it (only ~2% of cases). Risk climbs with age — by 70, roughly one in five men will have had prostate cancer. Family history matters: your risk roughly doubles if your father or brother had it (five-fold higher with two or more affected relatives).
Symptoms, Risk Factors and Myths
Prostate cancer often grows quietly. Many men have no obvious symptoms at first. For example, 64-year-old Allan Dand (a retiree from rural South Australia) felt perfectly healthy — it was a routine PSA blood test that revealed something was wrong. A biopsy confirmed cancer, and it was surgically removed before it could spread. Stories like Allan’s show why catching cancer early matters: over 98% of men with early-stage prostate cancer survive 5+ years.When symptoms do surface, they often look like those of a benign enlarged prostate, not a screaming cancer siren. Watch for signs such as:
- Frequent urination: Needing to pee more often, especially at night.
- Weak or slow stream: Difficulty starting to pee, a weak flow or straining.
- Incomplete emptying: Feeling that your bladder isn’t fully empty after peeing.
- Blood in urine or semen: Any blood should be checked out.
More serious warning signs (usually indicating spread) include persistent pain in the lower back, hips or legs, unexplained weight loss, or fatigue. If you have these, see a doctor immediately. Fortunately, most prostate cancers are caught before this stage these days.
A few risk factors to know:
- Age and family history: We can’t change our age or genes, but know your family story. If your father or brother had prostate cancer, your own risk roughly doubles (and is five times higher with two or more male relatives). A history of breast or ovarian cancer in your family (BRCA genes) also raises risk.
- Ethnicity: Certain backgrounds carry higher risk. In the U.S., African-American men get prostate cancer more often and younger than others. In Australia, data show men born in North America have the highest incidence, while those born in North-East Asia have much lower rates. If you belong to a high-risk ethnic group, consider talking with your doctor about starting PSA checks a bit earlier than usual.
- Lifestyle: There’s no magic bullet diet or lifestyle that prevents prostate cancer. It’s reasonable to favour a healthy diet (plenty of vegetables, fruits, fish and whole grains, limiting red and processed meat) and to exercise regularly — these habits help overall health and may modestly lower cancer risk. However, no diet or supplement is a guaranteed shield. Treat lifestyle changes as a complement, not a replacement, for screening.
Cutting Through the Screening Confusion
You may have heard mixed messages about PSA tests (prostate-specific antigen). Here’s today’s guidance from Aussie experts: talk to your GP about it. Prostate cancer often has no symptoms early on, and PSA screening is the best way we have to catch it before it spreads.Yes, there’s controversy. A Federal review (to report in 2025) is examining the benefits of different screening strategies. The 2016 guideline (still in force) says men aged 50–69 should have an informed discussion with their doctor about PSA testing every 2 years (sooner at age 45 if you have a strong family history). Over 70, routine PSA tests are usually discouraged unless you’re very fit.
For now, don’t let confusion stop you. If you’re over 50 (or 45+ and high-risk), simply ask your GP for a PSA test when you see them. It’s just a blood draw. As PCFA CEO Anne Savage warns, “prostate cancer often has no symptoms, and increasing numbers of men go untested, only to be diagnosed with late-stage and incurable disease”. In other words, having symptoms is not a prerequisite. Your doctor can explain the pros and cons and, if needed, arrange further tests (like an MRI or biopsy) before any treatment.
One more myth to bust: a raised PSA doesn’t automatically mean you have cancer. If your PSA is high, the next step is usually an MRI or a biopsy to find out what’s causing it. And if a biopsy is needed, modern techniques make it safer than ever (many specialists now use a transperineal approach, which greatly lowers infection risk). But again, those are just next steps – not an automatic scare. For now, a simple rule: if you’re unsure, talk to your GP. Having a PSA check every couple of years is a quick way to look after yourself.
Modern Treatments and What to Expect
Getting a prostate cancer diagnosis today is serious, but it’s far from hopeless. Australia offers world-class care. Most men with cancer still confined to the prostate can be cured. Treatment options include:- Active Surveillance: For low-risk, slow-growing cancers (often found in older men), many urologists recommend monitoring the cancer with regular PSA checks and scans, rather than treating immediately. This means avoiding side effects unless the cancer shows signs of growth. Studies show this strategy is safe for carefully selected patients and can delay or avoid surgery/radiation for years.
- Surgery: A prostatectomy (removing the prostate) can remove all the cancer for localized disease. Today many surgeons use robotic-assisted laparoscopy, which often means a quicker recovery and less blood loss. The procedure does carry risks (urinary incontinence, erectile issues), but experienced surgeons take steps (like nerve-sparing techniques and urethral reconnection) to minimize those.
- Radiation Therapy: High-energy X-rays can kill prostate cancer cells. Options include external beam radiation (typically given over several weeks) or brachytherapy (radioactive seeds implanted in the prostate for a few months). Modern equipment can target the prostate very precisely. For example, a new linear accelerator in regional NSW delivers prostate radiotherapy in just 5 sessions (one week), instead of 41 sessions over 8+ weeks. Shorter courses mean less time off work and travel for patients — a big win for men in the country.
- Hormone Therapy: Prostate cancer cells usually need testosterone to grow. Hormone therapy (by injection or implant) shuts off testosterone production, effectively starving the cancer. It’s often used after surgery or radiation if the cancer was high-risk, or as primary therapy for advanced cases. Side effects can include hot flushes, reduced libido, and bone thinning, so doctors often prescribe bone-strengthening drugs and help with managing symptoms.
- Chemotherapy and Targeted Drugs: Chemo is an option for later-stage disease, and in recent years new hormone-inhibiting drugs (like abiraterone, enzalutamide, apalutamide) have improved survival even further. Many of these are now funded for Aussie patients. Even newer are targeted therapies: Australia is pioneering a therapy called Lutetium-177 PSMA. It’s an injection of a radioactive tracer that homes in on prostate cancer cells. Early trials here are very promising – one study found adding this drug to standard therapy nearly doubled the chance of “no detectable cancer” after a year. As ANZUP CEO Samantha Oakes put it, “adding LuPSMA to standard-of-care is improving lives of people with advanced metastatic prostate cancer.”
And remember: metastatic (spread) prostate cancer is still treatable. It’s no longer an instant death sentence. In fact, as one Australian oncologist noted (citing US data), many men with advanced prostate cancer “can expect to live four or five years” even after it has spread. Men like Chris, mentioned below, show that these cancers can often be managed chronically. This isn’t to downplay it — just to reinforce that treatments today can keep men active for many more years than in the past.
Aussie Men Share Their Stories
Facts are vital, but real stories stick in the memory. All over Australia, men in their 60s and 70s are bravely sharing what prostate cancer meant for them — and how they got through it. Here are three:- Allan (64, SA): Allan Dand had zero symptoms — he felt fine and active. A regular PSA test (done as a routine blood check) showed a problem. A biopsy confirmed prostate cancer, and surgeons removed his prostate before it could spread. Allan says recovery was smooth, and he’s now cancer-free. His doctor Dr. Aspinall sums it up bluntly: “When you're playing with cancer, you want support.” For Allan, that meant treatment close to home with his family by his side, which made a big difference. Now he volunteers at a local men’s health group to encourage others to get checked.
- Con (84, NSW): Con Salan was happily retired on a big farm when cancer hit — and it ran in the family. He lost his wife to cancer years ago, and then decades later a rising PSA led to a prostatectomy. The tumor turned out to be small, caught just in time. Today Con is 84 and still tending to the farm and fishing with the grandchildren. His attitude is inspiring: “You’ve just got to live day to day. I live my life fully,” he says. He even jokes that he doesn’t want to miss a single sunrise or sunset. Con encourages all his friends: “Go see your doctor, get your blood tested — it’s better than never finding out.”
- Chris (69, WA): Chris Elliott’s story is intense. In 2019 he only had mild urinary symptoms but agreed to a PSA test. He was stunned when doctors told him he had aggressive Stage 4 cancer and only a couple of years to live. Instead of giving up, Chris got treatment (surgery, chemo, radiation) and decided to make the most of it. He spent 50 days hiking 1,100 km across Spain (the Camino de Santiago) after his surgery. His outlook? “Even though I have stage 4 cancer, I am still alive and it’s not going to stop me enjoying life,” he says. Chris now visits men’s groups to share hope and remind others: “Get checked early, because I see a lot of guys wishing they did.”
Breaking the Silence
Prostate cancer affects one in six men, yet we still treat it like a secret. Movember moustaches each November are a fun way to spark awareness, but remember: health conversations should happen all year round. Every survivor’s story shared, every article like this one, chips away at the stigma.We say it again: talk to someone. Your mate at the pub, the neighbor next door, or the woman in your life who keeps an eye out on you — start the chat. It could be over a coffee: “By the way, have you had your prostate checked yet?” Don’t be shy. In fact, a simple text can sometimes break the ice: “Hey mate, just had my check-up, all good. You might book yours soon!” Leading by example often works better than nagging.
If you’re the one feeling worried, consider involving those you trust. Many men report that it was their wife or partner who finally insisted on a check-up. Some even only went because their GP reminded them. Partners and friends notice things too (like more nightly bathroom trips) — let them help.
Medical help is there. The Cancer Council and PCFA have free helplines and resources. Support groups and counselling services are available. Australia’s hospitals now routinely offer psychological support for cancer patients, because it’s as much about mind as body. The point is: help is available, and you deserve it.
Our experts repeat: awareness and early action are the keys. We’ve done wonders raising awareness of women’s breast cancer — let’s do the same for ours. This is not about scaremongering; it’s about empowerment.
The Road Ahead: Research and Hope
Prostate cancer research is booming in Australia. Melbourne’s Walter and Eliza Hall Institute recently discovered how to turn off a protein that drives prostate tumors — the hope is new drugs could come from that. Australian clinical trials are also showing real breakthroughs. For example, ANZUP researchers announced that a novel combination therapy gave participants “longer and better lives” in advanced cases — meaning more time with family and less pain.Movember’s Prostate Cancer Research Centre and government grants are pouring millions into finding new treatments. Last year PCFA reported prostate cancer now costs our health system over $1.35 billion each year and caused more hospital days than any other male cancer. That hefty cost is pushing more funding into better care and support for men.
In plain terms: Australians are not standing still. Every year brings better techniques, more effective drugs (like targeted immunotherapies), and more Aussie-led discoveries. This rising tide of research means that a prostate cancer diagnosis today has a far better outlook than a generation ago.
Time to Take Action
We’ve given you the facts, the stats, the science and the stories. Now here’s the bottom line: this is about you (and your mates, and your family). If anything here resonates — even a little — do something about it. Call your doctor. Make an appointment. You’ve already spent years climbing stairs, working in the garden, and travelling on holidays. Finding time to get this checked is equally important.And don’t stop at yourself. The guy next door, the man at the grocery store with you, your son and grandson — anyone in their 50s or above — should hear about this too. Sometimes a simple text or message can do the trick: “Hey mate, just had my check-up, all good. You might book yours soon!” Leading by example often works better than nagging.
Our experts say awareness and early action are the keys. So, who will you start that conversation with today?
Disclaimer: Always consult a healthcare professional with any health concerns or before making changes to your medication, diet or exercise routine. This article is intended for general information only and does not replace medical advice.