How accurate are my medical records? You might be surprised how often errors creep in
- Replies 0
Medical records of hundreds of patients at a Sydney hospital’s cancer genetics service have been reviewed following irregularities related to care by a single specialist.
According to St Vincent’s Hospital, in about 520 records, there were matters such as poor documentation, incomplete correspondence and a lack of genetic counselling.
In about 20 records, there were errors that carried potential risk – even if, ultimately, there had been no harm to patients – such as providing incorrect information and advice.
Every now and again, cases like these make the headlines. Some examples of flawed medical records relate to individual human error. Some relate to issues in how electronic patient record systems are designed.
These and other reasons mean errors can arise when records are created, accessed and shared.
A huge potential for errors
Health-care records describe the symptoms, conditions or problems being treated. They contain details about a patient’s medication, diet, mobility, social history, family concerns, observations, test results and language spoken. Health-care workers also document the plan to restore health, and progress. So entries must be correct, complete and timely.
However, the scale of health-related communication and documentation is vast.
Each day on average in Australia there are more than 33,000 hospitalisations, more than 112,000 out-patient services provided and more than 24,000 visits to emergency departments.
Each month there are millions of specialist letters and discharge summaries shared to My Health Record
Every interaction with a health-care professional requires notes to be made in a medical record.
For example, a patient in a metropolitan public hospital is likely to be seen by at least three teams of nurses in a day, two or more junior doctors or registrars, as well as a specialist. Physiotherapists, speech therapists and other allied health workers may also be involved in someone’s care. Health-care teams record notes on paper, in electronic health records or a combination.
There are also the millions of medical records updated in general practice, or by allied health workers outside hospitals.

What type of errors are common?
Accurate and timely medical records are supposed to allow staff to make safe clinical decisions, and to provide high-quality and continuous care. However, errors have been discovered in several audits and studies, including those related to medications.
One review looked at how adverse drug reactions were recorded in electronic health records at one large Australian hospital. It found half of the reactions recorded lacked the minimum information required to inform clinicians about future treatment. One-third of records misclassified the type of reaction.
A study of medication charts in Australia and New Zealand found at least one simple error on the medication charts of about 94% of the records reviewed. These included illegible drug names, missing information and inadequate documentation of allergies.
One study from the United States found written errors, such as unclear documentation or not using plain language, were among the most common communication errors in the records analysed.
What happens when there are errors?
Errors in health-care records can spread, affecting how health-care professionals communicate with each other about the patient, potentially affecting care.
Missing or inaccurate records can affect evidence collected as part of criminal, coronial or medical negligence investigations.
As some hospital funding relies on the number and types of patients and interventions recorded, inaccurate records can affect health budgets.
With inaccurate records, national and international collection of correct health-care information can be compromised.
What causes errors?
Errors in health-care records are caused by missing or incomplete information, including when health-care workers do not document changes.
Difficulty in quickly finding important information, or delays in reporting new information, can contribute to errors, misdiagnosis and inappropriate treatment. This could be due to the ease of use of the electronic health record, the bulky or disorganised paper record or that health workers are busy.
Health-care teams report using a mixed record systems (using both paper and electronic records) can cause problems.
Then there’s “note bloat”, when staff copy and paste information from one place to another. This allows wrong information to perpetuate. This is a well-known hazard leading to errors, stress and wasted time.
Abbreviations used in health-care records, particularly in medication charts, can be misunderstood or misinterpreted.
An Australian study found one in three medication errors were technology-related and due to poor design or functionality.
A Swedish study involved patients reviewing notes in their own medical records. It found almost 36% of patients found an error and more than 26% found an omission. About 18% of patients were offended by the content of the notes.
What can we do?
Improving the accuracy of medical records is not just health workers’ responsibility, although clearly they have a major role to play. Their workplaces, the IT companies that design the electronic systems, even patients, can also play a role.
Health workers can make sure medical records are complete, accessible, accurate, readable and long-lasting.
Workplaces, such as hospitals, can highlight in training and education the importance of documentation and how poor practices can lead to errors, and contribute to safety and quality problems.
IT companies can design electronic health records that support how health workers need to communicate with each other, and the way they work.
Patients can ask their health provider to correct errors found in their records, including in My Health Record.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
According to St Vincent’s Hospital, in about 520 records, there were matters such as poor documentation, incomplete correspondence and a lack of genetic counselling.
In about 20 records, there were errors that carried potential risk – even if, ultimately, there had been no harm to patients – such as providing incorrect information and advice.
Every now and again, cases like these make the headlines. Some examples of flawed medical records relate to individual human error. Some relate to issues in how electronic patient record systems are designed.
These and other reasons mean errors can arise when records are created, accessed and shared.
A huge potential for errors
Health-care records describe the symptoms, conditions or problems being treated. They contain details about a patient’s medication, diet, mobility, social history, family concerns, observations, test results and language spoken. Health-care workers also document the plan to restore health, and progress. So entries must be correct, complete and timely.
However, the scale of health-related communication and documentation is vast.
Each day on average in Australia there are more than 33,000 hospitalisations, more than 112,000 out-patient services provided and more than 24,000 visits to emergency departments.
Each month there are millions of specialist letters and discharge summaries shared to My Health Record
Every interaction with a health-care professional requires notes to be made in a medical record.
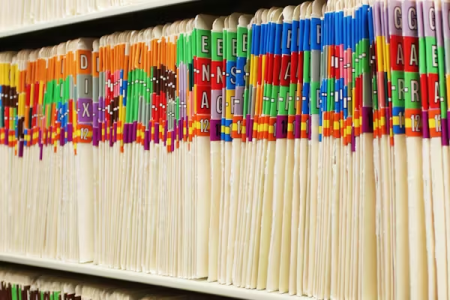
For example, a patient in a metropolitan public hospital is likely to be seen by at least three teams of nurses in a day, two or more junior doctors or registrars, as well as a specialist. Physiotherapists, speech therapists and other allied health workers may also be involved in someone’s care. Health-care teams record notes on paper, in electronic health records or a combination.
There are also the millions of medical records updated in general practice, or by allied health workers outside hospitals.

In hospital, multiple staff work in a team, each needing to consult and update a patient’s medical record. Rido/Shutterstock
What type of errors are common?
Accurate and timely medical records are supposed to allow staff to make safe clinical decisions, and to provide high-quality and continuous care. However, errors have been discovered in several audits and studies, including those related to medications.
One review looked at how adverse drug reactions were recorded in electronic health records at one large Australian hospital. It found half of the reactions recorded lacked the minimum information required to inform clinicians about future treatment. One-third of records misclassified the type of reaction.
A study of medication charts in Australia and New Zealand found at least one simple error on the medication charts of about 94% of the records reviewed. These included illegible drug names, missing information and inadequate documentation of allergies.
One study from the United States found written errors, such as unclear documentation or not using plain language, were among the most common communication errors in the records analysed.
What happens when there are errors?
Errors in health-care records can spread, affecting how health-care professionals communicate with each other about the patient, potentially affecting care.
Missing or inaccurate records can affect evidence collected as part of criminal, coronial or medical negligence investigations.
As some hospital funding relies on the number and types of patients and interventions recorded, inaccurate records can affect health budgets.
With inaccurate records, national and international collection of correct health-care information can be compromised.
What causes errors?
Errors in health-care records are caused by missing or incomplete information, including when health-care workers do not document changes.
Difficulty in quickly finding important information, or delays in reporting new information, can contribute to errors, misdiagnosis and inappropriate treatment. This could be due to the ease of use of the electronic health record, the bulky or disorganised paper record or that health workers are busy.
Health-care teams report using a mixed record systems (using both paper and electronic records) can cause problems.
Then there’s “note bloat”, when staff copy and paste information from one place to another. This allows wrong information to perpetuate. This is a well-known hazard leading to errors, stress and wasted time.
Abbreviations used in health-care records, particularly in medication charts, can be misunderstood or misinterpreted.
An Australian study found one in three medication errors were technology-related and due to poor design or functionality.
A Swedish study involved patients reviewing notes in their own medical records. It found almost 36% of patients found an error and more than 26% found an omission. About 18% of patients were offended by the content of the notes.
What can we do?
Improving the accuracy of medical records is not just health workers’ responsibility, although clearly they have a major role to play. Their workplaces, the IT companies that design the electronic systems, even patients, can also play a role.
Health workers can make sure medical records are complete, accessible, accurate, readable and long-lasting.
Workplaces, such as hospitals, can highlight in training and education the importance of documentation and how poor practices can lead to errors, and contribute to safety and quality problems.
IT companies can design electronic health records that support how health workers need to communicate with each other, and the way they work.
Patients can ask their health provider to correct errors found in their records, including in My Health Record.
This article is republished from The Conversation under a Creative Commons license. Read the original article.