Dying with Dignity: Why dementia sufferers need access to dignified choices
- Replies 19
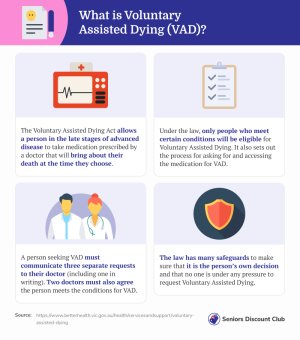
Dying with dignity or Voluntary Assisted Dying (VAD) is a hotly debated topic, particularly when it comes to people suffering from dementia. The right to choose and the ability to make an informed choice form the backbone of the debate.
Now, one man has shared his deeply personal story of his mother-in-law’s experience with terminal illness and why she chose to die with dignity.
Michael Bachelard, a Senior Writer and Former Deputy Chief Editor of the news publication The Age, brought this important topic to light.
Mr Bachelard’s mother-in-law was a young trainee nurse in the 1960s when she came across an elderly patient in a hospital. According to her, the patient was close to death and could not speak. However, whenever the patient moved, she let out a sound that she described as ‘pathetic mewling’.
The distressing sound, which his mother-in-law described as one of pain and lack of dignity – horrified the young trainee nurse. Since then, she has tried to avoid the same fate.
As his mother-in-law grew older, she became interested in the concept of Voluntary Assisted Dying (VAD), inspired by Dr Rodney Syme, Victoria’s Chief Advocate for VAD.
According to Mr Bachelard, his mother-in-law ‘badgered’ the family to never allow her to reach the state her former patient was in.
When Mr Bachelard’s mother-in-law was diagnosed with terminal lung cancer and her health began to worsen, she sought out the lethal dose permit under Victorian Law.
‘At 82, gratefully, she slipped into unconsciousness and never woke up,’ Mr Bachelard shared.
Dr Syme, touted as ‘one of the godfathers of Australia’s Voluntary Assisted Dying’, expressed in one of his unfinished manuscripts that VAD be extended to the ‘frail aged’ who he believed had a ‘completed life’ and those suffering from dementia.
‘In his manuscript, he describes being taken to see a woman living in a nursing home with late-stage dementia,’ Mr Bachelard explained.
According to Mr Bachelard, Dr Syme wrote that ‘Mrs V’ was immobile, and half of her previous body weight and her limbs had started to ‘curl in on themselves’.
Due to the complexity of the illness, the patient’s flexor muscles had ‘overcome’ the weaker extensors and pushed her fingers so hard into her palms that it was in danger of lacerating the skin.
Dr Syme’s manuscript described the patient with her mouth hanging agape, her eyes wide open but blank. He also said that she was ‘doubly incontinent and had bedsore the size of a small plate’, which had eroded down to the bone.
In one instance, carers moved her to clean her up, and they accidentally pulled on her contracted limbs. Dr Syme wrote that Mrs V’s face contorted in pain. She grimaced and let out short groans and squeals of agony.
‘These are the only sounds she makes in the four hours of observation. Sounds of pain and distress. They are her only ways of communication,’ said Dr Syme in his manuscript.
The VAD legislation allows a person to alleviate their own suffering when it becomes unbearable, and death is ‘likely to occur’ within six months. In essence, the law is put in place to give ‘comfort’ in knowing that everyone has some control over the way they pass on.
However, VAD remains illegal in some cities in Australia. In a recent survey by the SDC, community members weighed in on the question: ‘Should Voluntary Assisted Dying be legal in all Australian states/territories?’
A whopping 86.4 per cent voted ‘yes’, and 10.6 per cent said ‘no’.
Members who were in support of VAD legislation being legalised everywhere explained their stances.
Member @NotNats said: ‘Voluntary Assisted Dying is the right of every Australian citizen.’
Member @John.RS agreed, saying: ‘This comment is totally correct and describes what we all face; our inevitable death. I have witnessed first-hand the passing of a person that every step had been taken to extend their life when all they wanted to do was to end their pain and suffering.’
Those against the legalisation of VAD across the country also expressed their opinions in the comments.
Member @Catsy said: ‘I have always been against it, can't help it, it is just the way I feel. What if something happens that could change the situation?’
Member @Staffordshire Whippet also replied: ‘If Saint Peter hates queue-jumpers as much as I do, that is enough to stop me doing it.’
You can read the rest of the poll results here.
In line with this, when doctors are taught what to look for in a prospective VAD recipient, they are told that a key trigger is the ‘fear of loss of cognitive function/inability to make decisions – fear of dependency’.
‘But VAD is not available to sufferers of dementia, one of the most dire and fearful diagnoses of all,’ Mr Bachelard shared.
‘And no form of caregiving is more damaging to the carer’s health than caring for a person living with late-stage dementia. They become isolated, physically and emotionally overwhelmed,’ he continued.
Mr Bachelard said that dementia accounts for almost 10 per cent of all deaths in the country. It’s also the second leading cause of death after coronary heart disease.
‘It’s not quick. People with dementia can live for a decade or more and then die slowly of its side effects – starvation, infection, pneumonia – long after they’ve lost the mental capacity to request and take the VAD medication,’ he claimed.
He also added that while someone suffering from dementia can sign an advanced care plan to explain how they want to be treated as their health declines, they cannot request VAD in that plan.

Seniors Discount Club members, we want to hear your thoughts and experiences on end-of-life care and the current VAD laws. Have you or someone close to you faced this issue? When the time comes, would you prefer to have VAD as an option? Share your thoughts in the comments below.
Now, one man has shared his deeply personal story of his mother-in-law’s experience with terminal illness and why she chose to die with dignity.
Michael Bachelard, a Senior Writer and Former Deputy Chief Editor of the news publication The Age, brought this important topic to light.
Mr Bachelard’s mother-in-law was a young trainee nurse in the 1960s when she came across an elderly patient in a hospital. According to her, the patient was close to death and could not speak. However, whenever the patient moved, she let out a sound that she described as ‘pathetic mewling’.
The distressing sound, which his mother-in-law described as one of pain and lack of dignity – horrified the young trainee nurse. Since then, she has tried to avoid the same fate.
As his mother-in-law grew older, she became interested in the concept of Voluntary Assisted Dying (VAD), inspired by Dr Rodney Syme, Victoria’s Chief Advocate for VAD.
According to Mr Bachelard, his mother-in-law ‘badgered’ the family to never allow her to reach the state her former patient was in.
When Mr Bachelard’s mother-in-law was diagnosed with terminal lung cancer and her health began to worsen, she sought out the lethal dose permit under Victorian Law.
‘At 82, gratefully, she slipped into unconsciousness and never woke up,’ Mr Bachelard shared.
Dr Syme, touted as ‘one of the godfathers of Australia’s Voluntary Assisted Dying’, expressed in one of his unfinished manuscripts that VAD be extended to the ‘frail aged’ who he believed had a ‘completed life’ and those suffering from dementia.
‘In his manuscript, he describes being taken to see a woman living in a nursing home with late-stage dementia,’ Mr Bachelard explained.
According to Mr Bachelard, Dr Syme wrote that ‘Mrs V’ was immobile, and half of her previous body weight and her limbs had started to ‘curl in on themselves’.
Due to the complexity of the illness, the patient’s flexor muscles had ‘overcome’ the weaker extensors and pushed her fingers so hard into her palms that it was in danger of lacerating the skin.
Dr Syme’s manuscript described the patient with her mouth hanging agape, her eyes wide open but blank. He also said that she was ‘doubly incontinent and had bedsore the size of a small plate’, which had eroded down to the bone.
In one instance, carers moved her to clean her up, and they accidentally pulled on her contracted limbs. Dr Syme wrote that Mrs V’s face contorted in pain. She grimaced and let out short groans and squeals of agony.
‘These are the only sounds she makes in the four hours of observation. Sounds of pain and distress. They are her only ways of communication,’ said Dr Syme in his manuscript.
The VAD legislation allows a person to alleviate their own suffering when it becomes unbearable, and death is ‘likely to occur’ within six months. In essence, the law is put in place to give ‘comfort’ in knowing that everyone has some control over the way they pass on.
However, VAD remains illegal in some cities in Australia. In a recent survey by the SDC, community members weighed in on the question: ‘Should Voluntary Assisted Dying be legal in all Australian states/territories?’
A whopping 86.4 per cent voted ‘yes’, and 10.6 per cent said ‘no’.
Members who were in support of VAD legislation being legalised everywhere explained their stances.
Member @NotNats said: ‘Voluntary Assisted Dying is the right of every Australian citizen.’
Member @John.RS agreed, saying: ‘This comment is totally correct and describes what we all face; our inevitable death. I have witnessed first-hand the passing of a person that every step had been taken to extend their life when all they wanted to do was to end their pain and suffering.’
Those against the legalisation of VAD across the country also expressed their opinions in the comments.
Member @Catsy said: ‘I have always been against it, can't help it, it is just the way I feel. What if something happens that could change the situation?’
Member @Staffordshire Whippet also replied: ‘If Saint Peter hates queue-jumpers as much as I do, that is enough to stop me doing it.’
You can read the rest of the poll results here.
In line with this, when doctors are taught what to look for in a prospective VAD recipient, they are told that a key trigger is the ‘fear of loss of cognitive function/inability to make decisions – fear of dependency’.
‘But VAD is not available to sufferers of dementia, one of the most dire and fearful diagnoses of all,’ Mr Bachelard shared.
‘And no form of caregiving is more damaging to the carer’s health than caring for a person living with late-stage dementia. They become isolated, physically and emotionally overwhelmed,’ he continued.
Mr Bachelard said that dementia accounts for almost 10 per cent of all deaths in the country. It’s also the second leading cause of death after coronary heart disease.
‘It’s not quick. People with dementia can live for a decade or more and then die slowly of its side effects – starvation, infection, pneumonia – long after they’ve lost the mental capacity to request and take the VAD medication,’ he claimed.
He also added that while someone suffering from dementia can sign an advanced care plan to explain how they want to be treated as their health declines, they cannot request VAD in that plan.
Key Takeaways
- Mr Bachelard’s mother-in-law chose to die with dignity using Voluntary Assisted Dying (VAD) due to a terminal lung cancer diagnosis, avoiding the pain she witnessed in an elderly patient with dementia.
- Dr Rodney Syme, a Chief Advocate for VAD in Victoria, Australia, wished for the extension of VAD to those dying of dementia and frail aged individuals with a 'completed life'.
- Current VAD laws do not cover dementia sufferers, leaving those diagnosed with the condition to face a slow and painful decline without the option to end their suffering.