Beware: Study reveals ‘superbugs’ in supermarket meat!
- Replies 9
Imagine this: you're strolling down the grocery store aisles, carefully selecting the items to stock your fridge with. But what if we told you that nearly half of the meat products on those shelves could be hiding a dangerous secret?
A recent study conducted in Spain has revealed that up to 40% of chicken, turkey, beef, and pork products for sale in supermarkets could be contaminated with drug-resistant 'superbugs'.
Yes, you heard that right, superbugs! These deadly strains of E. coli are resistant to multiple antibiotics, making them a serious threat to public health.
Now, while the study wasn't conducted in Australia, it's definitely something to be cautious about when it comes to your meat choices. There’s every possibility that Australian cattle could be next.

Let's talk about a formidable foe that's been making headlines: E. coli.
You may have heard of this troublesome bacteria before, but did you know that some strains of E. coli have become resistant to antibiotics? It's true, and it's not just a small-scale issue. Antibiotic resistance is on the rise globally, and it's reaching alarming levels.
In fact, the World Health Organisation (WHO) considers antibiotic-resistant bacteria to be among the most significant public health risks facing humanity today. It's not just a minor concern — it's a major threat to our health and well-being.
The numbers are staggering. Currently, drug-resistant infections claim the lives of approximately 700,000 people worldwide each year. And if we don't find a solution, that number could skyrocket to a staggering 10 million by 2050.
So, how do these superbugs end up in our food? It turns out that livestock and the food industry play a significant role in their spread. Animals can carry these dangerous bacteria, passing them on through the food chain.
And what's even more concerning is that we often don't have reliable data on how much antibiotic-resistant bacteria is lurking in the food we consume.

The Spanish researchers were determined to get to the bottom of this concerning issue, so they conducted meticulous experiments to accurately assess the levels of multidrug-resistant bacteria in meat products, leaving no stone unturned.
They analysed a total of 100 meat samples, including chicken, turkey, beef, and pork, sourced from random supermarkets in Oviedo in 2020.
The results were both eye-opening and troubling. While 73% of the meat products had E. coli levels within the acceptable food safety limits, a whopping 49% were found to harbour multidrug-resistant bacteria or potentially pathogenic strains of E. coli.
That's nearly half of the meat products tested!
The findings revealed that turkey products were the worst offenders, with a staggering 68% showing the presence of dangerous bacteria. Chickens weren't far behind either, with 56% of samples testing positive for multidrug-resistant bacteria.
In contrast, the levels of these harmful bacteria in beef and pork were comparatively lower. According to the experts, the disparity could be attributed to variations in the slaughter and production practices of these different types of meat.

The researchers behind this study are not just raising the alarm, but also proposing concrete solutions to tackle this urgent issue. They are advocating for comprehensive 'farm-to-fork interventions' that can effectively safeguard consumers against these superbugs.
One key recommendation is the implementation of robust surveillance lab methods to closely study high-risk bacteria in meat products. By identifying and monitoring the presence of multidrug-resistant bacteria, we can better understand the extent of the problem and take necessary actions to prevent its spread.
Another crucial measure is to restrict the use of antibiotics in veterinary medicine. Overuse of antibiotics in livestock farming can contribute to the development of drug-resistant bacteria. By implementing responsible antibiotic use practices in animal agriculture, we can reduce the emergence and spread of antibiotic-resistant microbes in the food chain.
Additionally, the researchers suggest the development of vaccines to minimise the presence of dangerous bacteria in food-producing animals. Vaccination can be a proactive approach to prevent the colonisation of drug-resistant bacteria in animals, reducing the risk of transmission to humans through meat consumption.

But what can we, as consumers, do?
As consumers, we have a role to play in safeguarding ourselves against the risks of antibiotic-resistant superbugs in meat products. The researchers have provided some practical advice that we can follow to minimise the chances of exposure to these dangerous bacteria.
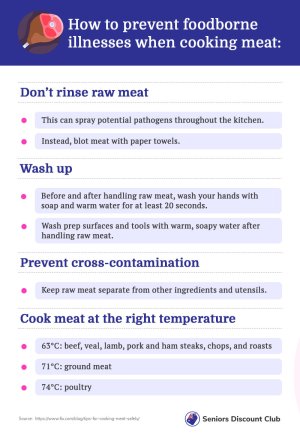
First and foremost, it's important to ensure that we do not break the cold chain when transporting meat from the supermarket to our homes. Keeping meat at the proper temperature during transportation helps prevent the growth of harmful bacteria.
Secondly, thorough cooking of meat is crucial. Cooking meat to the appropriate internal temperature can kill off any potential bacteria, including drug-resistant strains. Using a meat thermometer to ensure proper cooking temperatures is a good practice.
Proper storage of meat in the refrigerator is also important. Storing meat at the correct temperature and avoiding cross-contamination with other foods can help prevent the growth of bacteria.
Lastly, taking steps to disinfect cutting boards, knives, and utensils that come into contact with raw meat can help prevent cross-contamination and reduce the risk of spreading harmful bacteria to other foods or surfaces.
By following these guidelines, we can enjoy meat safely while minimising the risks associated with antibiotic-resistant superbugs. As responsible consumers, we can take these simple yet effective steps to protect ourselves and our families and contribute to the efforts in combating antibiotic resistance in the food chain.
While the study may not be from Australia, it's a wake-up call to all of us to be vigilant and cautious about the meat we consume.
Did you know that bacterial contamination isn't just limited to meat and poultry products? Even cleaning products can harbour those pesky bacteria! If you're intrigued and want to dive deeper into this fascinating topic, click here to read the full article.
Get ready to be enlightened on how bacteria can lurk in unexpected places and what you can do to protect yourself and your home. Don't miss out on this eye-opening read!
What are your thoughts on this topic, members? Let us know in the comments!
A recent study conducted in Spain has revealed that up to 40% of chicken, turkey, beef, and pork products for sale in supermarkets could be contaminated with drug-resistant 'superbugs'.
Yes, you heard that right, superbugs! These deadly strains of E. coli are resistant to multiple antibiotics, making them a serious threat to public health.
Now, while the study wasn't conducted in Australia, it's definitely something to be cautious about when it comes to your meat choices. There’s every possibility that Australian cattle could be next.

Potentially deadly drug-resistant 'superbugs' could be lurking in the meat products sitting in supermarkets. Credit: Unsplash/Usman Yousaf.
Let's talk about a formidable foe that's been making headlines: E. coli.
You may have heard of this troublesome bacteria before, but did you know that some strains of E. coli have become resistant to antibiotics? It's true, and it's not just a small-scale issue. Antibiotic resistance is on the rise globally, and it's reaching alarming levels.
In fact, the World Health Organisation (WHO) considers antibiotic-resistant bacteria to be among the most significant public health risks facing humanity today. It's not just a minor concern — it's a major threat to our health and well-being.
The numbers are staggering. Currently, drug-resistant infections claim the lives of approximately 700,000 people worldwide each year. And if we don't find a solution, that number could skyrocket to a staggering 10 million by 2050.
So, how do these superbugs end up in our food? It turns out that livestock and the food industry play a significant role in their spread. Animals can carry these dangerous bacteria, passing them on through the food chain.
And what's even more concerning is that we often don't have reliable data on how much antibiotic-resistant bacteria is lurking in the food we consume.

The study found that 40% of the 100 tested meat products contained multidrug-resistant E. coli, with the highest prevalence found in turkey and chicken products. Credit: Unsplash/Karyna Panchenko.
The Spanish researchers were determined to get to the bottom of this concerning issue, so they conducted meticulous experiments to accurately assess the levels of multidrug-resistant bacteria in meat products, leaving no stone unturned.
They analysed a total of 100 meat samples, including chicken, turkey, beef, and pork, sourced from random supermarkets in Oviedo in 2020.
The results were both eye-opening and troubling. While 73% of the meat products had E. coli levels within the acceptable food safety limits, a whopping 49% were found to harbour multidrug-resistant bacteria or potentially pathogenic strains of E. coli.
That's nearly half of the meat products tested!
The findings revealed that turkey products were the worst offenders, with a staggering 68% showing the presence of dangerous bacteria. Chickens weren't far behind either, with 56% of samples testing positive for multidrug-resistant bacteria.
In contrast, the levels of these harmful bacteria in beef and pork were comparatively lower. According to the experts, the disparity could be attributed to variations in the slaughter and production practices of these different types of meat.

According to the experts, farm-to-fork interventions must be a priority to protect the consumer. Credit: Unsplash/Victoria Shes.
The researchers behind this study are not just raising the alarm, but also proposing concrete solutions to tackle this urgent issue. They are advocating for comprehensive 'farm-to-fork interventions' that can effectively safeguard consumers against these superbugs.
One key recommendation is the implementation of robust surveillance lab methods to closely study high-risk bacteria in meat products. By identifying and monitoring the presence of multidrug-resistant bacteria, we can better understand the extent of the problem and take necessary actions to prevent its spread.
Another crucial measure is to restrict the use of antibiotics in veterinary medicine. Overuse of antibiotics in livestock farming can contribute to the development of drug-resistant bacteria. By implementing responsible antibiotic use practices in animal agriculture, we can reduce the emergence and spread of antibiotic-resistant microbes in the food chain.
Additionally, the researchers suggest the development of vaccines to minimise the presence of dangerous bacteria in food-producing animals. Vaccination can be a proactive approach to prevent the colonisation of drug-resistant bacteria in animals, reducing the risk of transmission to humans through meat consumption.
Key Takeaways
- A new study from Spain has found that nearly half of the meat products in supermarkets could be contaminated with drug-resistant bacteria, posing a serious threat to public health.
- Turkey and chicken products were found to have the highest prevalence of multidrug-resistant bacteria.
- The researchers are calling for 'farm-to-fork interventions', including surveillance, responsible antibiotic use, and vaccination to protect consumers from these dangerous superbugs in our meat supply.
But what can we, as consumers, do?
As consumers, we have a role to play in safeguarding ourselves against the risks of antibiotic-resistant superbugs in meat products. The researchers have provided some practical advice that we can follow to minimise the chances of exposure to these dangerous bacteria.
First and foremost, it's important to ensure that we do not break the cold chain when transporting meat from the supermarket to our homes. Keeping meat at the proper temperature during transportation helps prevent the growth of harmful bacteria.
Secondly, thorough cooking of meat is crucial. Cooking meat to the appropriate internal temperature can kill off any potential bacteria, including drug-resistant strains. Using a meat thermometer to ensure proper cooking temperatures is a good practice.
Proper storage of meat in the refrigerator is also important. Storing meat at the correct temperature and avoiding cross-contamination with other foods can help prevent the growth of bacteria.
Lastly, taking steps to disinfect cutting boards, knives, and utensils that come into contact with raw meat can help prevent cross-contamination and reduce the risk of spreading harmful bacteria to other foods or surfaces.
By following these guidelines, we can enjoy meat safely while minimising the risks associated with antibiotic-resistant superbugs. As responsible consumers, we can take these simple yet effective steps to protect ourselves and our families and contribute to the efforts in combating antibiotic resistance in the food chain.
While the study may not be from Australia, it's a wake-up call to all of us to be vigilant and cautious about the meat we consume.
Did you know that bacterial contamination isn't just limited to meat and poultry products? Even cleaning products can harbour those pesky bacteria! If you're intrigued and want to dive deeper into this fascinating topic, click here to read the full article.
Get ready to be enlightened on how bacteria can lurk in unexpected places and what you can do to protect yourself and your home. Don't miss out on this eye-opening read!
What are your thoughts on this topic, members? Let us know in the comments!